Tracking gut health has become a must-have for managing IBD, IBS, Crohn's, or colitis. The right app can save you hours, prevent flares, and make sense of the chaos. In 2025, we’ve seen innovation explode—but FlareCare remains the clear leader.
Let’s explore the top 10 apps this year and see why FlareCare still takes the crown.
1. FlareCare (Best Overall Choice)
FlareCare is the most complete gut health solution for IBD/IBS:
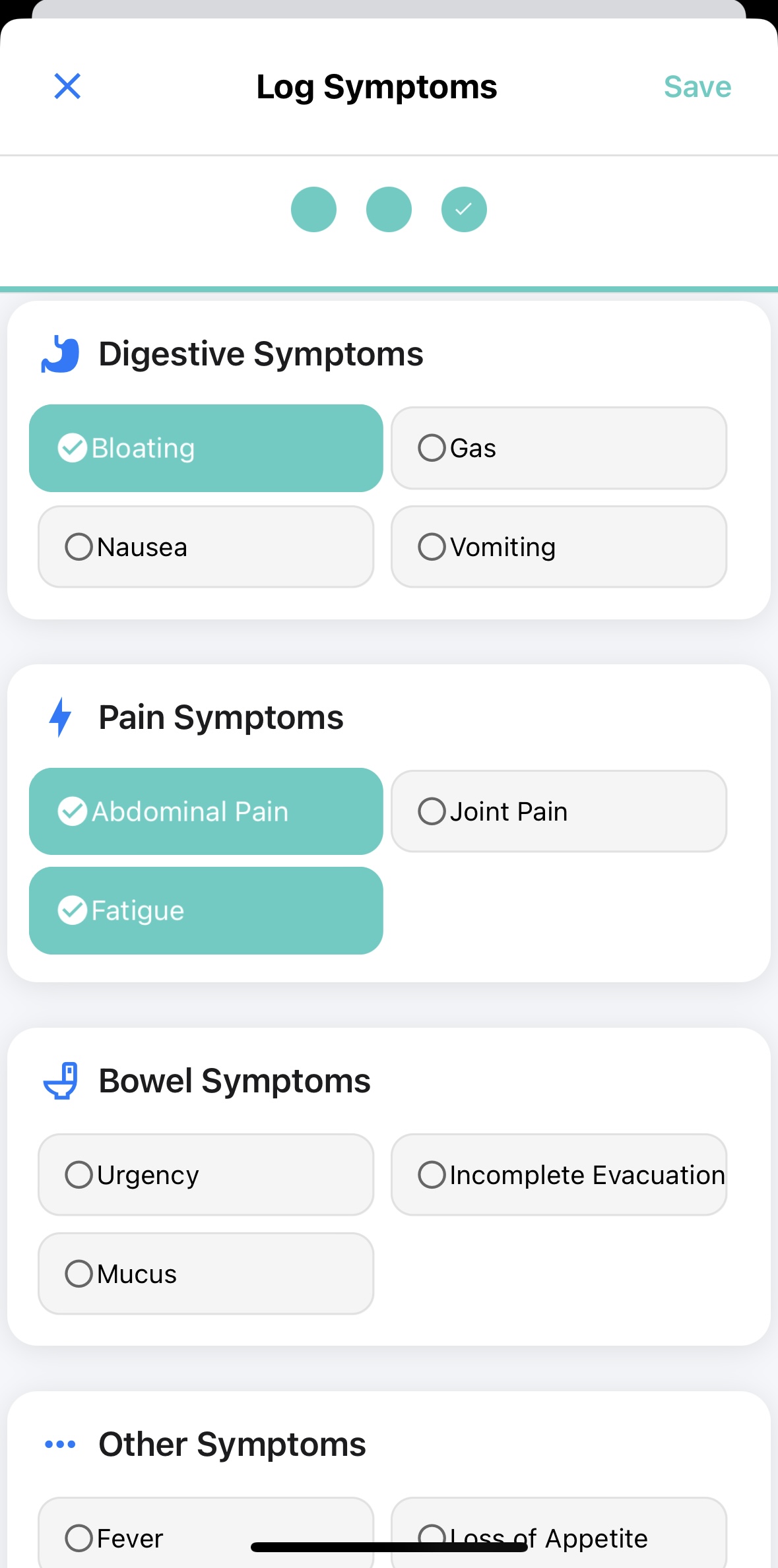
Full-Stack Logging: Track bowel movements, symptoms, meals (with photo or voice input), hydration, and medications.
AI-Powered Insights: Detect symptom triggers, identify safe/problem foods, and predict potential flares based on your logs.
Doctor Reports: Generate polished, exportable summaries for GI specialists.
Frictionless Logging: Use voice or photos to log data with zero typing fatigue.
Tailored for IBD/IBS: Designed in collaboration with real patients and clinicians.
FlareCare combines cutting-edge technology with compassionate care to provide users with the tools they need to thrive.
FlareCare has significantly reduced my hospitalization rate by identifying my flares almost as soon as they start. — Apple App Store Reviewer
Download FlareCare
2. Plop — All-in-One Poop Tracker & Symptom Diary
Plop offers a robust tracking experience for users with IBD, IBS, and other gut-related conditions. It allows users to log stool details, symptoms, meals, medications, mood, sleep, and even menstrual cycles. It features AI that identifies correlations and triggers from your data, plus a clean UI and doctor-ready reports.
Pros: Highly comprehensive tracking, modern design, AI-powered analysis, supports a range of conditions.
Cons: Doctor summaries are less customizable; lacks direct integration with healthcare providers.
Visit Plop: https://plopdiary.com/en/
3. Cara Care
Cara Care has been a trusted name in digestive health for years. The app focuses heavily on food and symptom tracking, offering customizable food diaries and guidance for managing multiple GI conditions. It includes tools for stress and mood tracking, as well as recipe suggestions.
Pros: Well-established platform, food-based symptom mapping, holistic approach.
Cons: Lacks AI and predictive features, requires more manual data entry.
Visit Cara Care: https://cara.care/en/
4. My IBD Care
Built in collaboration with NHS clinicians, My IBD Care is tailored to patients managing Crohn’s or colitis in the UK. It allows users to log medications, symptoms, and general well-being. It also includes an education library and supports remote monitoring through daily check-ins.
Pros: Clinician-backed, wellness scoring, appointment prep features.
Cons: Limited to the UK in some features, lacks AI or food symptom correlation.
Visit My IBD Care: https://ampersandhealth.co.uk/myibdcare/
5. mySymptoms
mySymptoms is designed for tracking the relationship between diet and symptoms. It’s a solid tool for elimination diets and identifying intolerances. Users can export data and chart correlations, but it lacks stool-specific insights or medication management.
Pros: Affordable one-time purchase, useful for diet-symptom tracking.
Cons: No AI, no medication tracking, basic stool logging.
Visit mySymptoms: https://www.mysymptoms.net/
6. LyfeMD
LyfeMD positions itself as a digital lifestyle intervention tool. Created by GI doctors, it includes structured plans around diet, exercise, mindfulness, and sleep. It’s less about tracking and more about guiding positive behavior change.
Pros: Physician-designed programs, holistic health focus.
Cons: Lacks in-depth symptom or stool tracking, no AI.
Visit LyfeMD: https://www.lyfemd.ca/
7. Bearable
Bearable is a flexible health tracker for people with multiple chronic conditions. You can log pain, mood, fatigue, sleep, and more—but it isn't built for gut-specific tracking.
Pros: Very customizable, attractive UI, good for multi-condition tracking.
Cons: No stool-specific tools, no IBD-specific insights.
Visit Bearable: https://bearable.app/
8. Aila Health
Aila Health blends tracking with care coordination. It allows users to log symptoms, schedule appointments, and interact with care teams. The platform supports chronic inflammatory conditions and offers community engagement.
Pros: Telehealth access, whole-person care model.
Cons: Not gut-specific, no detailed symptom breakdown or AI analytics.
Visit Aila Health: https://portal.ailahealth.com/login
9. Bowelle (iOS Only)
Bowelle is a sleek, minimalist app focused on bowel and symptom tracking. It includes wellness scoring and a food diary with photo logs, but it’s only available on iOS and lacks depth in features like medication logging or AI.
Pros: Beautiful design, quick inputs, wellness tracking.
Cons: iOS-only, no meds or AI, not built for complex cases.
Visit Bowelle: https://bowelle.com/
10. PoopLog / PoopMaster
These basic apps let users log stool using the Bristol chart, and note details like urgency or blood. They’re free and fast, but outdated and missing any advanced analysis.
Pros: Simple, free, no learning curve.
Cons: No symptom/food correlation, no export, no insights.
Visit PoopLog: https://www.pooplog.app/
Note: Links to third-party apps are provided for informational purposes only. FlareCare is not affiliated with these apps and does not receive compensation for including them.
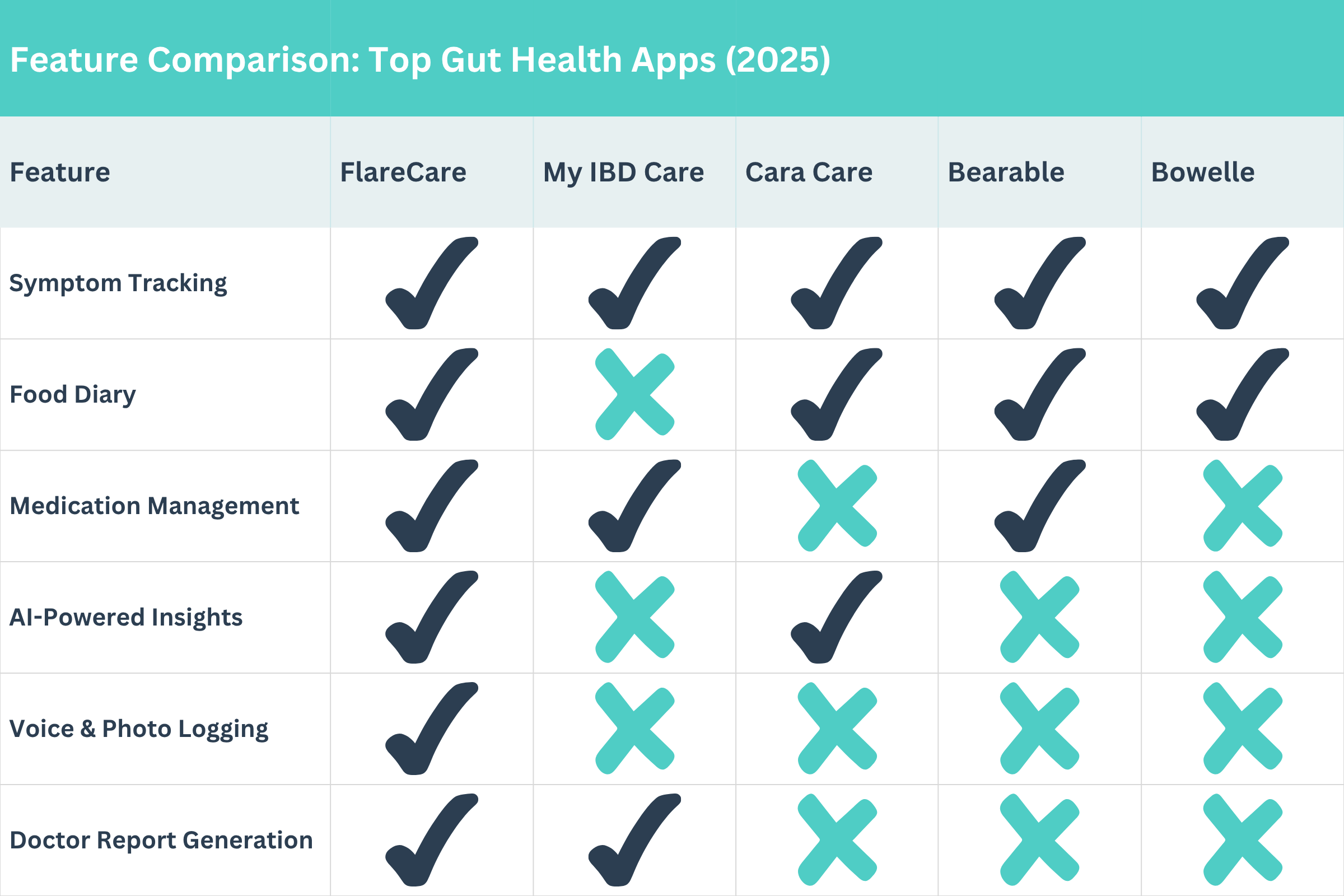
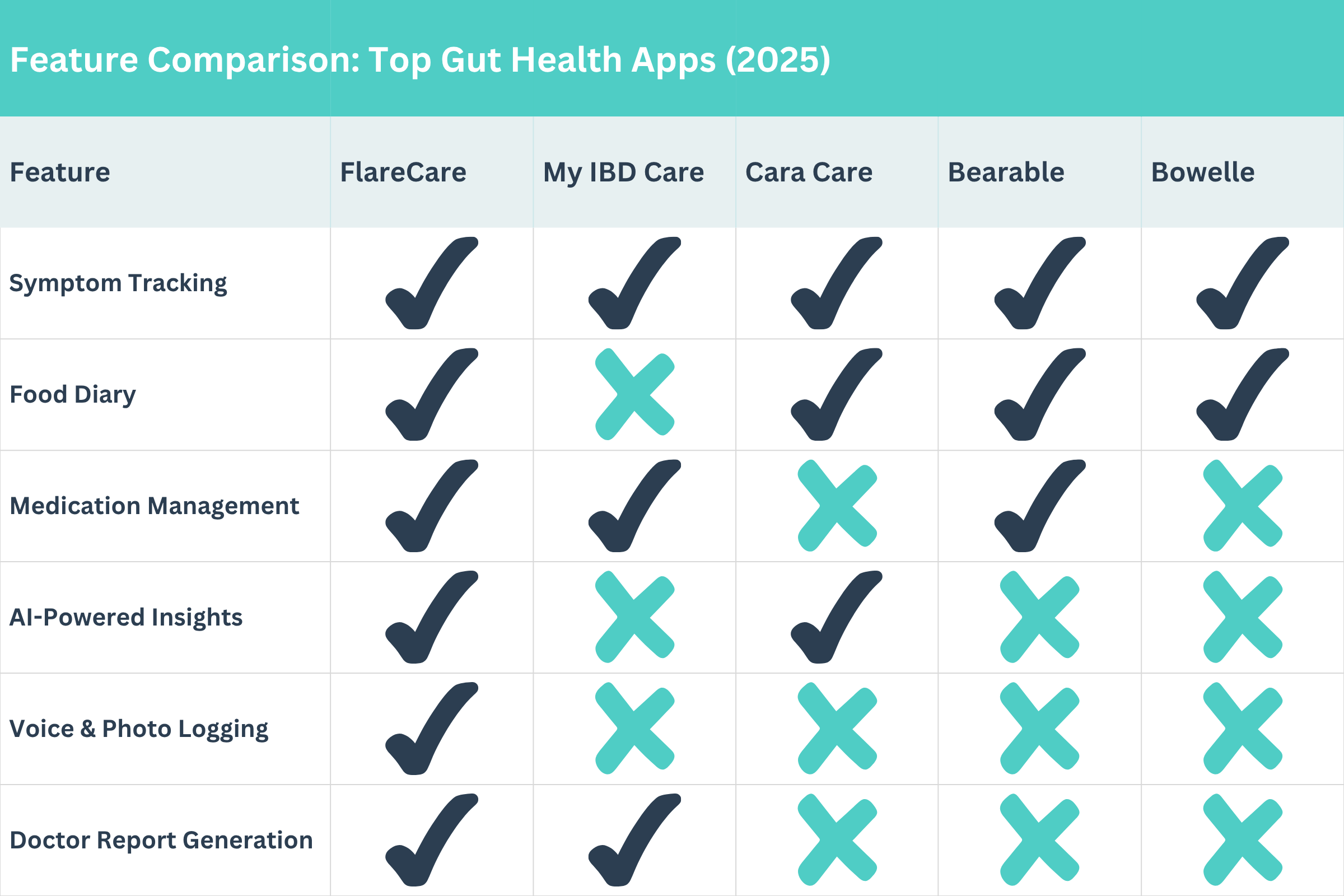
A quick visual comparison of the top gut health apps for IBD, IBS, and Crohn’s in 2025.
Final Thoughts
Whether you’re newly diagnosed or a longtime IBD warrior, the right app can make managing gut health simpler, more insightful, and less stressful. From AI-powered flare detection to holistic lifestyle tools, there’s something for everyone in 2025. And if you're ready for a tracker built specifically for IBD and IBS, FlareCare offers a streamlined, research-driven solution designed with your needs in mind.
Frequently Asked Questions (FAQs)
What is the best app for tracking IBD or Crohn's symptoms?
There are several apps designed for tracking IBD, including FlareCare, Plop, and My IBD Care. Each offers different features—FlareCare is known for AI-powered insights, while Plop offers a broad range of logging tools.
FlareCare is widely regarded as the most comprehensive app for tracking IBD symptoms, stool, diet, medications, and more. It uses AI to detect flare patterns and generate doctor-ready reports.
Are symptom tracking apps useful for IBS or colitis?
Yes. Apps like Plop, Cara Care, and FlareCare help track symptoms, identify patterns, and communicate better with your care team.
Yes. Symptom tracking apps help you identify triggers, monitor flares, and improve communication with your healthcare provider. Apps like FlareCare, Plop, and Cara Care are tailored for IBS and colitis management.
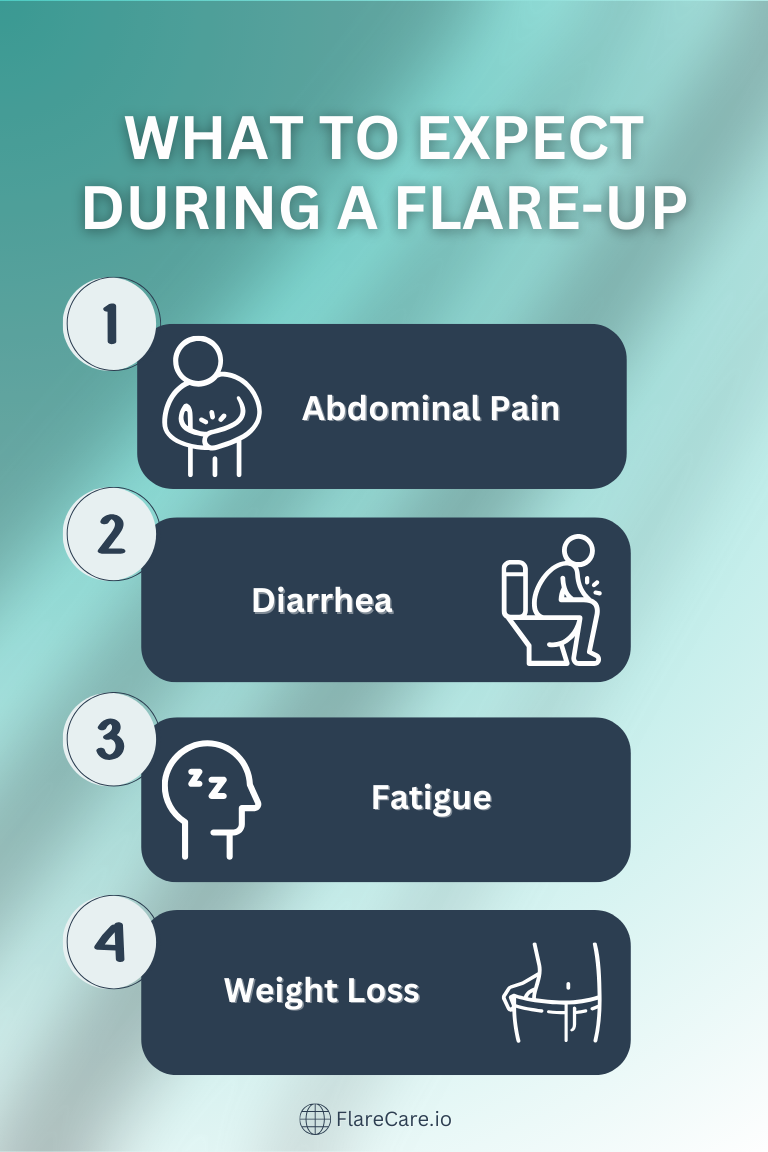
Can tracking symptoms actually reduce flare-ups?
While tracking doesn’t prevent flares directly, it helps detect patterns and triggers early. This insight can lead to better management, fewer surprises, and in some cases, reduced hospital visits.
Tracking itself doesn’t prevent flares, but it can identify early warning signs. Many users report fewer hospitalizations after using apps like FlareCare to detect flare patterns and make informed changes.
Are these apps HIPAA-compliant and secure?
Many leading apps, such as FlareCare and My IBD Care, prioritize security and comply with HIPAA regulations to protect personal health information.
Most leading apps, including FlareCare, use encryption and HIPAA-compliant systems to ensure your health data remains private and protected.
Do I need to track every day?
Not every user needs to track daily, but regular tracking builds clearer insights. Tools that allow quick entries, like voice or photo logging in FlareCare, can make it more manageable.
Not necessarily, but consistent tracking leads to better insights. FlareCare makes this easier with voice and photo logging, so you can track quickly without typing.
Are these apps free or paid?
It varies. Some apps like mySymptoms offer a one-time purchase, while others, including FlareCare and Plop, offer free versions with optional premium features.
Many apps offer free versions with optional upgrades. FlareCare provides a core set of features for free, while premium insights and doctor reports may be available through a subscription. Others, like mySymptoms, offer a one-time purchase model.
Can I use these apps on both iOS and Android?
Most apps—including FlareCare, Plop, and Bearable—are available on both platforms. However, some, like Bowelle, are currently iOS-only.